Beyond Stenosis: CT-Identified Plaque Types Aid in Identifying Ischemic Lesions
January 13, 2015
RELATED LINKS
 FDA Approves Software for Noninvasive Cardio Studies
FDA Approves Software for Noninvasive Cardio Studies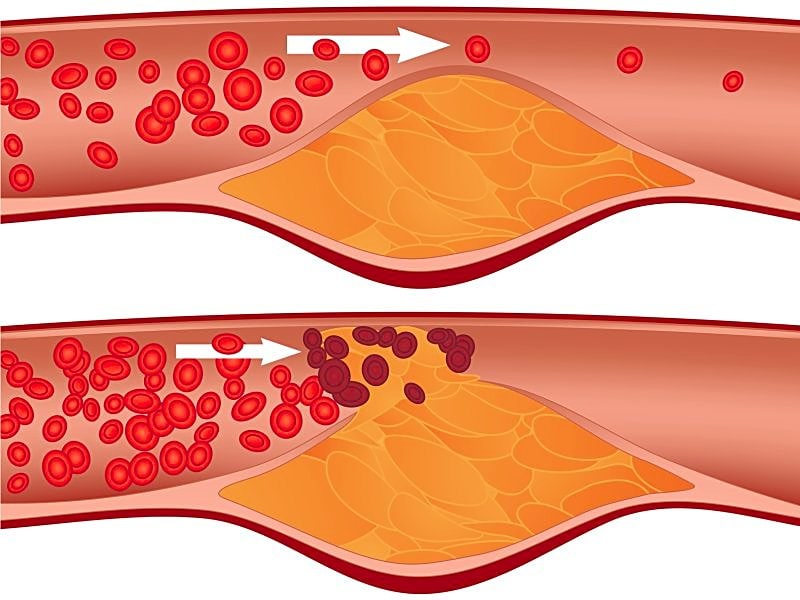 Predicting Plaque Rupture in CAD: Review Lists Risky Signs
Predicting Plaque Rupture in CAD: Review Lists Risky Signs
FFR-CT and iFR Accurately Identify Coronary Stenoses
Topic Alert
Receive an email from Medscape whenever new articles on this topic are available.
![]() Add Atherosclerosis to My Topic Alert
Add Atherosclerosis to My Topic Alert
DRUG & REFERENCE INFORMATION
Coronary CT Angiography
Pediatric Supravalvar Aortic Stenosis
Atherosclerotic Disease of the Carotid Artery
NEW YORK, NY — Anatomical characteristics of atherosclerotic plaque help provide additional information beyond the extent of coronary stenosis in the prediction of ischemia in patients with stable coronary artery disease, according to the results of a new study[1].
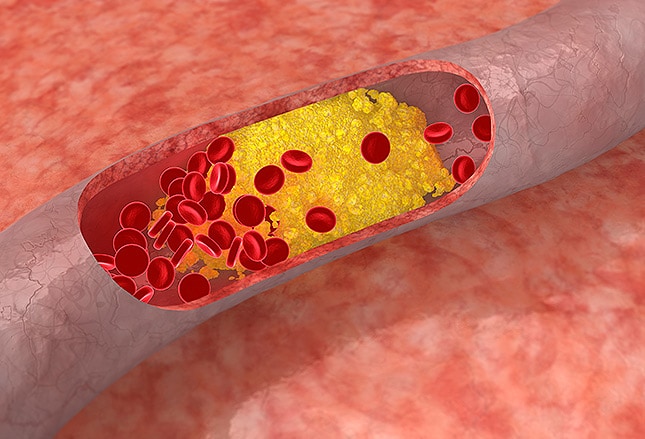
In a study performed in 252 stable patients, positive arterial remodeling and the presence of a necrotic lipid-rich core, which were both assessed using computed tomography (CT) angiography, were associated with coronary lesions that cause ischemia, report investigators.
Senior investigator Dr James Min (Weill Cornell Medical College, New York) said the study was designed to help researchers understand the underlying atherosclerotic plaque characteristics and what these physiologic parameters mean to ischemia in patients with symptomatic coronary disease. The simple paradigm of “stenosis vs no stenosis” for identifying ischemic lesions is clearly insufficient, so their aim has been to understand the various morphologic features of the coronary plaque, features that serve as surrogate markers for the underlying physiology within the coronary artery, he said.
“And that physiology can be something as general as a transition or transformation of the coronary atherosclerotic plaque or it may represent measures of the local environment, such as endothelial dysfunction,” Min told heartwire .
The study, which was published January 12, 2015 in JACC: Cardiovascular Imaging with first author Dr Hyung-Bok Park (Weill Cornell Medical College), included stable patients with coronary artery disease undergoing invasive coronary angiography and CT angiography. Lesion ischemia was assessed using fractional flow reserve (FFR) during invasive angiography and performed for 407 coronary lesions. With CT angiography, a lesion was considered obstructive if the coronary stenosis was 50% or greater.
The researchers assessed specific adverse characteristics of the atherosclerotic plaque: aggregate plaque volume (%); positive remodeling; low-attenuation plaque, which served as a marker of the necrotic lipid-laden plaque core; and microcalcifications. The microcalcifications are difficult to see by CT given the spatial-resolution limitations, so investigators used intraplaque spotty calcification as a surrogate. These measures, explained Min, have been previously documented in pathologic and prior CT studies to be “prognostically implicated in acute coronary syndrome.”
Compared with nonischemic lesions, those that caused ischemia had a greater stenosis, longer length, larger plaque volume, higher aggregate plaque volume, higher rates of positive remodeling, low-attenuation plaque, and spotty calcification. In a multivariate analysis, obstructive stenosis, lesion length, positive remodeling, and low-attenuation plaque were associated with ischemia, but spotty calcification was not.
“What we found was that the spotty calcifications actually weren’t that strongly predictive,” Min said. “Positive arterial remodeling, however, and to a certain degree low-attenuation plaque, added to the prediction of whether or not a specific plaque caused ischemia.”
When investigators stratified the lesions by stenosis, positive remodeling was a predictor of ischemia for all lesions, but aggregate plaque volume and low-attenuation plaque were associated only with ischemia for lesions with >50% stenosis, the conventional threshold for determining whether a lesion is angiographically severe.
