Coronary Calcium Scores Can Help Some ‘Intermediate-Risk’ Patients Avoid Statins:More Evidence
Larry Hand
September 26,2016
RELATED LINKS
 Moderate Tea Drinking May Reduce CAC Scores,CV Events:MESA
Moderate Tea Drinking May Reduce CAC Scores,CV Events:MESA
 No Coronary Calcium in 50% of Statin-Eligible Patients:MESA
No Coronary Calcium in 50% of Statin-Eligible Patients:MESA
 Coronary Artery Calcification Predicts All-Cause Mortality
Coronary Artery Calcification Predicts All-Cause Mortality
ESSEN,GERMANY — Obtaining coronary artery calcium (CAC) scores in addition to performing guideline-recommended procedures can improve stratification of patients as high or low risk for coronary events,whether on statin therapy or not,according to a new study involving a German primary-prevention cohort [1].
CAC scoring could help clinicians match risk-factor modification to atherosclerotic plaque burden and actual risk,and it could lead to avoiding therapy in low-risk patients with low 10-year event rates,researchers say.
“Especially in subjects with intermediate risk according to traditional risk factors and a recommendation for statin therapy according to current guidelines,CAC scoring may help to identify patients without coronary plaque burden who have a low future event rate,in whom lifelong statin therapy may not be needed,” lead author Dr Amir A Mahabadi (University of Disburse-Essen,Essen,Germany) told heartwire from Medscape.
Mahabadi and colleagues conducted a study involving 3745 individuals in the Ruhr area who were recruited during 2000–2003 into the Heinz Nixdorf Recallstudy.
The results were published online September 21,2016 in JACC:Cardiovascular Imaging.
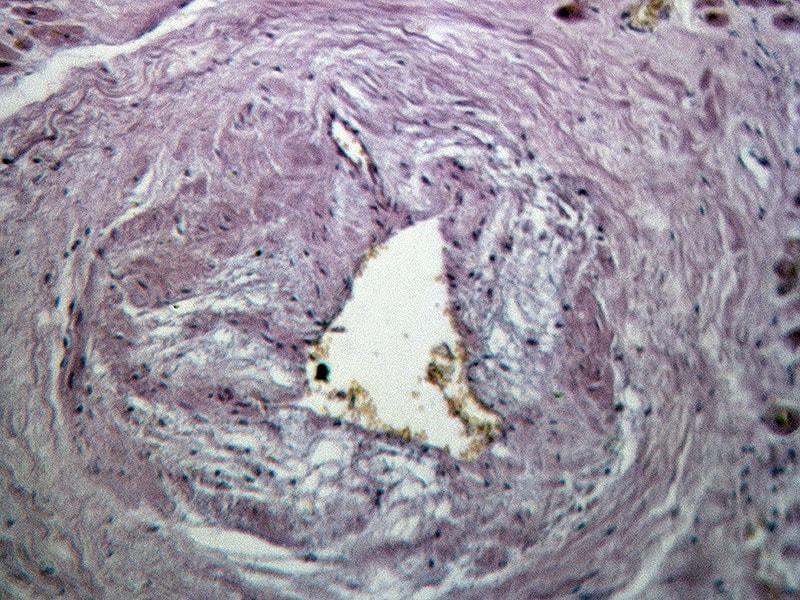
The researchers used electron-beam computed tomography (CT) to obtain images from the right pulmonary artery to the apex. They defined CAC as a focus of at least 4 contiguous pixels with a CT density greater than 130 Hounsfield units. Physicians and patients were blinded to the baseline CAC score.
Their first goal was to quantify differences among participants for statin therapy when applying guideline recommendations of the American Heart Association/American College of Cardiology (AHA/ACC) vs European Society of Cardiology (ESC) guidelines. AHA/ACC guidelines have a wider indication for statin therapy than ESC guidelines.
Of the 3745 individuals (mean age 59.8,53% female) all without lipid-lowering therapy or known cardiovascular disease,1288 (34.4%) met criteria for statin therapy under ESC guidelines,while 2101 (56.1%) did so under AHA/ACC guidelines. Also,897 (24%) met statin indication under AHA/ACC but not under ESC,while 84 (2.2%) met statin criteria under ESC only.
A total of 131 fatal or nonfatal MIs occurred during a mean follow-up of 10.4 years (event rate 3.5%),while 241 hard cardiovascular events occurred (event rate 6.43%). Sixty participants with coronary events did not fit statin indication under ESC,while only 19 events occurred among participants without statin indication under AHA/ACC.
The researchers found that participants with CAC scores of 400 or higher experienced a 10-fold higher event rate compared with participants with a CAC score of zero (event rate 12.6% vs 1.3%). Frequency of events was low (3.3% or lower) in participants whose CAC score fell below 100.
“Following AHA/ACC vs ESC guidelines for statin therapy leads to relevantly different recommendations regarding statin therapy in primary prevention,” Mahabadi told heartwire. “However,according to both guidelines,frequency of zero or low CAC score in patients with statin recommendation is high,while this group has an overall low event rate. Our results show that if CAC score is applied to appropriate subgroups,this may lead to significant improvement of risk prediction,especially in addition to European recommendations.”
Strong Evidence for Use
Dr Michael Blaha (Johns Hopkins Ciccarone Center for the Prevention of Heart Disease,Baltimore,MD),who coauthored an accompanying editorial [2],told heartwire that with the current study,”We now have excellent evidence from four studies [1,3-5]showing that coronary artery calcium can further reclassify risk after the pooled cohort equations and that the primary advantage is identifying patients who are truly at low risk despite being statin eligible under the new ACC/AHA prevention guidelines.
“The overall evidence is definitely strong enough to use CAC as part of shared decision making with patients right now,” he added. “While this study is just one small piece of the puzzle,the totality of the evidence is now clear.
“We hope the next set of guidelines provides a thorough literature review on CAC and provides a clear and thoughtful recommendation about its use. Right now,the guidelines don’t exactly match the way clinicians are using CAC in practice. The guidelines need to catch up to the current state of CAC imaging and provide clear recommendations that will facilitate its coverage by major payers,” Blaha concluded.
The study was funded by the Heinz Nixdorf Foundation,the German Ministry of Education and Science (BMBF),and the Deutsche Forschungsgemeinschaft. The authors and editorialists reported no relevant financial relationships.
Follow Larry Hand on Twitter: @LarryHand16. For more from theheart.org,follow us on Twitterand Facebook.
