Emphysema-related COPD on CT signals higher malignancy risk
By Eric Barnes, AuntMinnie.com staff writer
Individuals who have certain types of emphysema may also be at higher risk of cancer if they have suspicious nodules found on CT lung cancer screening scans, according to new research. The findings could help researchers better determine which suspicious nodules warrant further workup.
The study of 817 participants in the National Lung Screening Trial (NLST) with CT-detected nodules examined CT-identified subtypes of chronic obstructive pulmonary disease (COPD). The researchers found an association between all emphysema-related COPD — particularly centrilobular emphysema (CLE) or paraseptal emphysema (PSE) — and malignancy.
“The presence of centrilobular emphysema or paraseptal emphysema … was associated with an increased risk of nodules as malignant,” said Dr. Caroline Chiles from Wake Forest Baptist Medical Center. The association increased with increasing severity of CLE, but there was no association with COPD severity as measured by spirometry. These findings should be incorporated into the lung cancer screening guidelines, Chiles added.
Looking for clues
As CT lung cancer screening programs evolve, researchers are looking to minimize the need for invasive workup by looking for clues that indicate a suspicious CT finding could be malignant or benign. Such characteristics can shape nodule management guidelines such as Lung-RADS and those from the Fleischner Society.
“The purpose of [our] analysis was to examine the association of CT-defined COPD subtypes with lung cancer diagnosis for participants in the National Lung Screening Trial,” Chiles said in a talk at the recent RSNA meeting in Chicago.

Dr. Caroline Chiles from Wake Forest Baptist Medical Center.
The case-controlled study from Wake Forest University and several other institutions consisted of 817 NLST participants, including 200 diagnosed with lung cancer during the trial. Another 617 individuals who were not diagnosed with lung cancer during the trial served as controls.
Eight readers, including seven thoracic radiologists and one pulmonologist, examined the presence and severity of CT-definable COPD phenotypes on low-dose CT lung cancer screening images.
“The readers looked for COPD features such as centralized lobular emphysema and bronchial wall thickening,” she said.
Each reader subclassified each scan as normal or as one of three phenotypes related to COPD: emphysema-predominant, airway-predominant, or mixed-pattern. They looked for centrilobular emphysema (trace, mild, or moderate), paraseptal emphysema, bronchial wall thickening, centrilobular nodularity, and interstitial fibrosis.
“Patients with moderate centrilobular emphysema had a greater distribution of these lucencies, and within this category we included patients who had both confluent areas of emphysema and advanced destructive emphysema with architectural distortion,” Chiles explained.
For mild paraseptal emphysema, the focus was on juxtapleural lucencies 1 cm or smaller; for those with moderate disease, the focus was on more substantial juxtapleural lucencies in the mediastinal region.
Emphysema confers higher risk
Emphysema-predominant COPD, particularly CLE and PSE, was associated with a higher risk of malignancy, while nonemphysema-predominant COPD and mixed emphysema showed no increased association with lung cancer, Chiles said.
| Association between COPD and malignancy risk | |||||
| Controls (no lung cancer) | % of total | Lung cancer cases | % of total | Odds ratio | |
| All subjects | 617 | 100% | 200 | 100% | Reference group |
| Any CLE | 396 | 64.18% | 148 | 74% | 1.59 |
| Any PSE | 211 | 34.20% | 84 | 42% | 1.39 |
| Emphysema-predominant COPD | 215 | 34.85% | 93 | 46.5% | 1.53 |
| Airway-predominant COPD | 162 | 26.26% | 46 | 23% | 1.00 |
| Mixed-pattern emphysema or airway-predominant COPD | 102 | 16.53% | 22 | 11% | 0.76 |
“We found that the presence of any level of emphysema was associated with a diagnosis of malignancy in these patients with indeterminate nodules,” Chiles said.
The odds ratios increased as the emphysema level increased from trace to mild to moderate, but there were too few cases of severe emphysema to be statistically significant, she added.
“We also saw this increase in patients with any level of paraseptal emphysema compared with no paraseptal emphysema,” Chiles said.
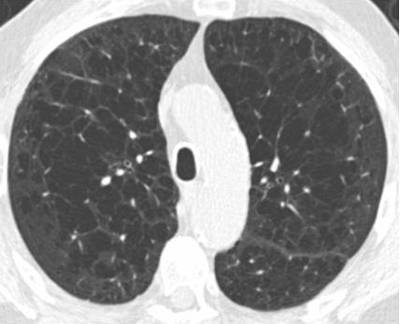
Above, patient with centrilobular emphysema; below, patient with paraseptal emphysema. Both COPD phenotypes were associated with malignancy in nodules 6 mm to 19 mm in diameter at CT lung cancer screening. Images courtesy of Dr. David Gierada and Dr. Caroline Chiles.

Factors not associated with emphysema were bronchial wall thickening at any level of severity (odds ratio, 0.92), centrilobular nodularity (odds ratio, 1.05), and pulmonary fibrosis (odds ratio, 1.05).
“Pulmonary fibrosis is known to be associated with malignancy, but we had too few cases to really demonstrate this association,” she said. “Only 37 patients had pulmonary fibrosis, and in all of our cases it was mild.”
Looking at spirometry results, the analysis did not reveal an association with malignancy (patients with airflow obstruction had an odds ratio of 1.12). Similarly, on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) scale for COPD severity, odds ratios for malignancy were all over the map and did not show a clear association.
The ramifications of these findings, although vague, “should be incorporated with nodule risk-prediction models to better show the association between individuals who are worthy of further workup when nodules are encountered on lung cancer screening,” she said.
In response to a question from the audience, she said that patients should definitely be told about CT findings of COPD.
“I think it can be helpful for patients and physicians to know about the presence of COPD, because they can help manage COPD better and reduce the number of visits to the emergency room — so I think it’s important to include the presence of COPD in the report,” Chiles said. “Whether we list it as a separate finding under Lung-RADS is a separate topic, and at this point I think it’s more about including it in the report than adding a code to Lung-RADS.”
