How to spot vaping-associated lung injury on imaging exams
By Kate Madden Yee, AuntMinnie.com staff writer
October 9, 2019 — Lung injury linked to electronic nicotine delivery systems — or vaping — is recognizable on medical imaging exams, and radiologists are key to identifying the condition, according to a clinical perspective published online October 8 in the American Journal of Roentgenology.
“Many patterns of lung injury have been reported with vaping,” wrote a team led by Dr. Travis Henry of the University of California, San Francisco (UCSF). “It is critical for the radiologist to recognize that [lung injury patterns] may be seen with vaping, and thus the radiologist may be the first person to prompt the clinical team to ask about relevant exposures.”
Because vaping is a relatively new phenomenon, there is no standardized case definition for vaping-associated injury, Henry and colleagues noted. A diagnosis of lung injury due to vaping therefore depends on determining an association between any change in vaping habits and the onset of lung disease, they wrote.
Electronic nicotine delivery systems encompass a range of devices, including vapes, electronic cigarettes (e-cigarettes), vape pens, vaporizers, hookah pens, e-pipes, “cigalikes,” e-hookahs, and tank systems, according to the authors. They listed a number of lung injuries associated with vaping, or the inhalation of an aerosolized liquid, and they outlined typical imaging findings for each:
- Hypersensitivity pneumonitis: Findings on CT include symmetric upper lung-predominant and midlung-predominant ground-glass opacity, poorly defined centrilobular nodules, and sometimes attenuation that suggests air trapping.
- Diffuse alveolar hemorrhage: Chest x-ray or CT alone is not enough to distinguish this condition from other causes of acute lung opacities such as aspiration, edema, or infection. However, patients with alveolar hemorrhage may be anemic, Henry and colleagues wrote. Bronchoalveolar lavage with “persistent or increasingly bloody” samples can confirm the diagnosis of this condition.
- Acute eosinophilic pneumonia: Often secondary to first-time vape usage, increased use, a brand change, or the resumption of traditional smoking products, recent cases have been difficult to diagnose due to nonspecific manifestations and the absence of peripheral eosinophilia at the time of presentation.
- Organizing pneumonia: This is characterized by fibroblast proliferation and collagen deposition, and typical CT findings are bilateral patchy ground-glass opacity, consolidation, or both in peripheral or perilobular distribution, according to the researchers.
- Lipoid pneumonia: Juices are the main flavoring agents for electronic nicotine delivery systems, but ingredients such as glycerin can cause endogenous phospholipidosis. “The presence of lipid-laden macrophages on bronchoalveolar lavage or foreign body reaction around lipid at histology can confirm diagnosis,” the group wrote.
- Giant cell interstitial pneumonia: Hard metal contamination of vaping aerosols is well documented, the authors noted. They encountered one case of this rare pneumonia, which was due to trace amounts of cobalt in the patient’s vape mechanism.
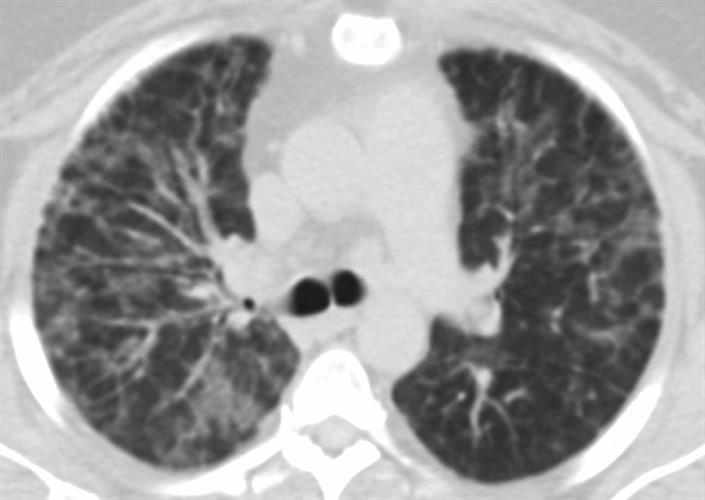
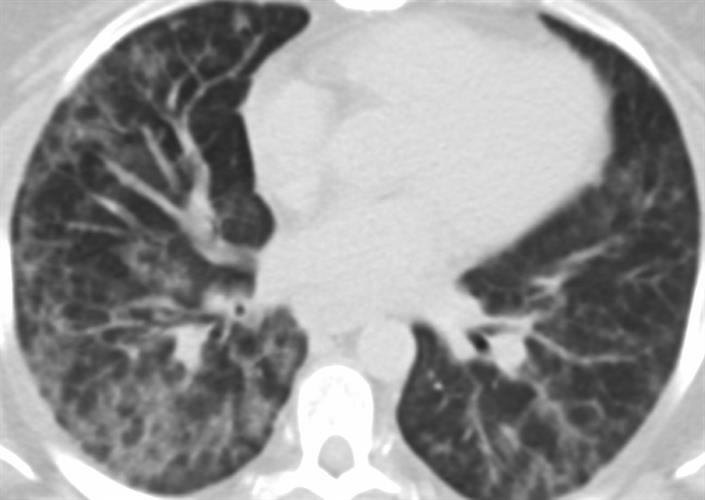
Giant cell interstitial pneumonia attributed to vaping in a 49-year-old woman who presented with one to two years of worsening dyspnea. Axial CT images show relatively symmetric ground-glass opacity and perilobular opacities involving all lobes. Subsequent surgical lung biopsy results were consistent with giant cell interstitial pneumonia. When asked about exposure, the patient said she had begun vaping a tetrahydrocannabinol (THC) mixture around the time her symptoms started. She had no other occupational exposures to heavy metals, and her vape pen was found to have traces of cobalt on subsequent analysis. Images courtesy of the American Roentgen Ray Society.
Radiologists are an important part of the clinical team when it comes to patients presenting with lung injury, the researchers concluded.
“When the radiologist sees one of these patterns … it is important to raise the possibility of vaping-induced lung injury because cessation of vaping is an important step in treatment,” they wrote.
